If you're interested in this topic, the first thing you should do is scroll down and download a copy of the review paper by Farrell and colleagues about the management of heritable genetic diseases in dogs (links below). And after you're done here, you should sit down and read it. All of it.
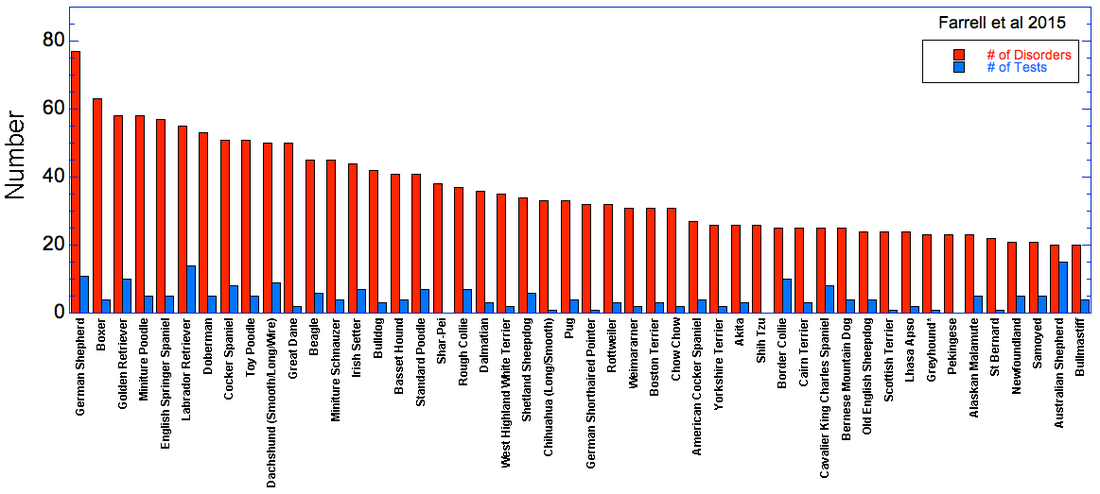
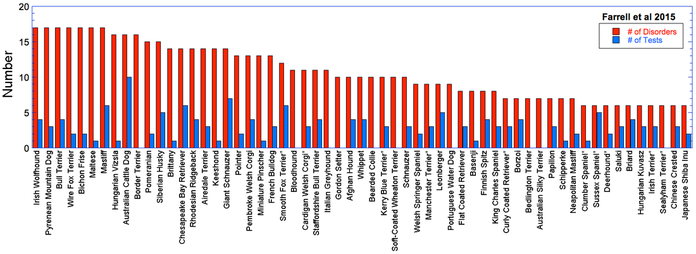
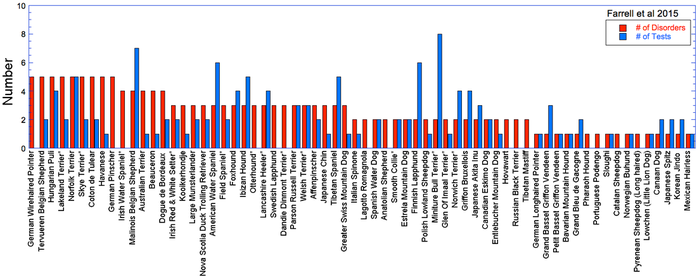
In the downloadable supplementary materials of the paper by Farrell and colleagues, there is a table with information about the number of identified disorders in more than 200 breeds of dogs, as well as the number of available tests. I've generated some graphs from these data, which I've split into breeds with more than 20 disorders (top) and breeds with fewer (bottom). The graphs are large and might be difficult to read here, so you can download copies to view at a larger size. I also provide a link to download a copy of the table on which they are based below.
- Farrell LL, JJ Shoenebeck, P Wiener, DN Clements, and K Summers. 2015. The challenges of pedigree dog health: approaches to combating inherited disease. Canine Genetics and Epidemiology 2:3; DOI 10.1186/s40575-015-0014-9 (pdf)
not an exhaustive list of all inherited disorders in pedigree dogs". In fact, the comprehensive online database of disorders in animals (OMIA, Online Mendelian Inheritance in Animals) lists 651 "traits and disorders" (as of 7 March 2015). To be fair, this includes some normal traits like coat color and genes for breed features like brachycephaly. But certainly the majority are veterinary disorders.
Perhaps a better indicator is the list in OMIA of "Mendelian trait / disorder, key mutation known"; i.e., there is a known gene associated with the trait. For this there are 188 listed, and even discounting a dozen or two as non-disease traits (like coat color), the list is still half again longer than the one used in the Farrell et al. study. Notably, it includes 16 types of progressive retinal atrophy, 26 different lysosomal storage diseases, and 23 heart disorders; those alone amount to 65.
Of course, because the OMIA database is comprehensive, many of the disorders listed are probably very rare. There really isn't any way to know what fraction of the dogs in a particular breed are diagnosed with any of these illnesses in their lifetime, so a list of hundreds of disorders that occur with trivial frequency isn't an accurate reflection of the prevalence of genetic disorders in general. On the other hand, most of the disorders on the Farrell et al. list are familiar to me, so they would not be from incidence reports of only a handful of dogs. Getting better data will require more comprehensive reporting and record-keeping than is regularly done in most countries, although some of the Scandinavian countries are keeping excellent records that might be useful for better analyses.
DNA tests are becoming less expensive, but they nevertheless can run into hundreds of dollars per dog in many breeds for just the relatively few ones available. Veterinary diagnostics can be much more expensive (e.g., hip radiographs, blood tests, holter monitors). Responsible breeders are diligent about taking advantage of available tests, but you have to wonder about the potential size of the bill if we had tests for even half the disorders in most breeds. There is clearly the possibility that the cost of testing could become prohibitive and breeders would be faced with some very difficult choices.
Perhaps most worrisome about these data is what they reveal about our notion of the "health tested" dog. Dogs are often advertised as health tested, but given the size of the gap between the number of known disorders and the number of available tests, this is clearly quite misleading. Breeders might wish for more DNA tests, but if each one potentially limits breeding options, at some point they will find themselves facing a genetic minefield across which it is impossible to find a clear path.
The genes for all of these genetic disorders are already out there; they have already affected some animal, which is how we know about them. If they are not now causing a noticeable problem, it is because they are rare, and they will not become a problem if they continue to stay rare. Testing for the (few) mutations we already have tests for does nothing to protect against the risk of some other mutation becoming a problem, and in fact DNA testing as it is widely used today might be reducing the number of affected animals for a known disorder but increasing the risk of producing animals afflicted with one caused by these known but rare mutations (as explained here). Every puppy contains copies of the mutations of its parents. Producing many puppies with the same mutations will cause rare mutations to become common, and some "new" genetic disorder will make an appearance in a breed when the frequency becomes high enough. Even if we had all the necessary DNA tests, they will never eliminate genetic disorders in dogs. There are hundreds of mutations we know about for which we have no test, and even more that we don't yet even know exist.
Farrell et al. make this key point:
"Doing a genetic test and subsequently eliminating an individual from the breeding population may not be the best strategy, as by targeting a particular allele at one genetic locus for removal from the gene pool of a particular breed, breeders may in fact increase allele frequencies of genetic variants on alternative haplotypes at the same, or a different locus, that are recessively deleterious. In addition, by eliminating some animals from breeding, a reduction in the effective population size will occur, thus risking higher levels of inbreeding, potential founder effects and genetic bottlenecks. in essence, by correcting one problem there is a chance of inadvertently creating a new one."
The game of genetic whack-a-mole could potentially go on forever.
If inappropriate breeding strategies like overuse of popular sires, inbreeding, and strong selection for particular traits is at the root of the problem, then the first and most useful step we can take is to stop doing those things. Since genetic disorders will be rare if the genes that cause them are rare, the most efficient way of managing genetic disorders in dogs should be adoption of the appropriate breeding strategies to accomplish this. We have not been doing this very well.
A "health tested" puppy with a coefficient of inbreeding of 30% is an oxymoron. Preventing the 25% risk of a known disorder, then breeding with a 30% risk of risk of producing a new one, is not a responsible breeding strategy, and certainly not the road to better canine health. Breeders should avail themselves of DNA tests, tools like estimated breeding values that will improve assessment of genetic risk, and be more open and honest about reporting genetic problems.
But none of these things will prevent or even reduce the overall level of genetic disorders unless breeders also adopt sensible, sustainable breeding strategies that keep the problematic mutations rare in the population and avoid the inbreeding that will bring two together in the same animal.
| Breeds with < 20 disorders |
| Breeds with > 20 disorders |
| Farrell et al 2015- Supplentary Table 1.pdf |
| farrell_et_al_2015_-_s2.pdf |
The data in the paper I talk about in this post is NOT intended to be a complete and exhaustive list of genetic disorders in dogs. They say that and I emphasize it as well, and I also provide the list both from this study and the current OMIA database so people can see what is included and what is not. The publication was not about the data in that table; it is a discussion of strategies for managing genetic disorders in dogs. The point I made with this information (which was otherwise buried in a large table in the unpublished supplementary materials) was that the gap between the number of genetic disorders and available tests is HUGE, and that using a more compete list would make this even worse.
Another note, added on 9 March:
Some people are apparently reading the comments below and somehow construing that DNA tests are a waste of time. They certainly are NOT, and this is not what I have said. DNA tests for disorders caused by single recessive mutations will completely eliminate the possibility of producing a puppy with a genetic disorder caused by that mutation. This is a certainty, and YES, breeders should do this.
The point made here is that there are many more known mutations for which we have NO DNA tests. We can't just ignore that these exist. DNA tests are not "health" tests, they are mutation tests. Doing all relevant DNA tests for a dog is not the equivalent of a "healthy dog" seal of approval, yet this is how the phrase "health tested" is interpreted by the lay person and potential puppy-buyer, and unfortunately also by many breeders.
The data here clearly show that in many breeds, there are many more known disorders for which we have NO tests. Molecular genetics can offer breeders no help in preventing these from becoming a problem because they don't know the cause. Clearly, if we don't have DNA tests, then we need breeding strategies that will minimize risks.
Farrell et al. point out that using DNA tests inappropriately can actually make things worse:
"Doing a genetic test and subsequently eliminating an individual from the breeding population may not be the best strategy, as by targeting a particular allele at one genetic locus for removal from the gene pool of a particular breed, breeders may in fact increase allele frequencies of genetic variants on alternative haplotypes at the same, or a different locus, that are recessively deleterious. In addition, by eliminating some animals from breeding, a reduction in the effective population size will occur, thus risking higher levels of inbreeding, potential founder effects and genetic bottlenecks. In essence, by correcting one problem there is a chance of inadvertently creating a new one."
There is NOTHING here that suggests that breeders should not be doing DNA tests. What the authors do say is that breeders must understand that appropriate BREEDING STRATEGIES are fundamental to controlling genetic disorders. DNA tests are an extremely valuable tool, but they are only available for a fraction of the known disorders, and used with inappropriate breeding strategies they can very well make things worse.
In case this is still not absolutely clear:
1) Breeders should avail themselves of DNA tests that will prevent genetic disorders;
2) BUT - preventing genetic disorders in dogs is not going to come from DNA testing without also using breeding strategies that appropriately manage genetic risk.
-------------------
*** "Population Genetics for Dog Breeders" starts 30 March ***
Visit our Facebook Groups
ICB Institute of Canine Biology
...the latest canine news and research
ICB Breeding for the Future
...the science of animal breeding
(Total = 188)
Achromatopsia (cone degeneration, hemeralopia), AMAL
Achromatopsia (cone degeneration, hemeralopia), GSPT
ACTH-independent adrenal Cushing syndrome, somatic
Alopecia, colour mutant
Amelogenesis imperfecta
Anhidrotic ectodermal dysplasia
Arrhythmogenic right ventricular cardiomyopathy
Ataxia, cerebellar
Ataxia, cerebellar, in Old English Sheepdogs and Gordon Setters
Ataxia, cerebellar, progressive early-onset
Ataxia, spinocerebellar
Autosomal dominant PRA
Black hair follicle dysplasia
Bleeding disorder due to P2RY12 defect
Brachycephaly
C3 deficiency
Cardiomyopathy, dilated
Cataract, early onset
Cerebellar abiotrophy
Cerebellar hypoplasia, VLDLR-associated
Chondrodysplasia
Chondrodysplasia, disproportionate short-limbed
Ciliary dyskinesia, primary
Cleft palate 1
Coat colour, agouti
Coat colour, albinism, oculocutaneous type IV
Coat colour, brown
Coat colour, dominant black
Coat colour, extension
Coat colour, grizzle
Coat colour, harlequin
Coat colour, melanistic mask
Coat colour, merle
Coat colour, saddle tan vs black-and-tan
Coat colour, white spotting
Coat colour, white spotting, due to KIT
Collie eye anomaly
Colorectal hamartomatous polyposis and ganglioneuromatosis
Cone-rod dystrophy 1
Cone-rod dystrophy 2
Cone-rod dystrophy 3
Cone-rod dystrophy 4
Cone-rod dystrophy, Standard Wire-haired Dachshund
Congenital keratoconjunctivitis sicca and ichthyosiform dermatosis
Craniomandibular osteopathy
Curly coat
Cystinuria, type I - A
Cystinuria, type II - A
Cystinuria, type II - B
Deficiency of cytosolic arylamine N-acetylation
Degenerative myelopathy
Dermoid sinus
Dwarfism, pituitary
Early retinal degeneration
Ectodermal dysplasia
Ectodermal dysplasia/skin fragility syndrome
Elliptocytosis
Epidermolysis bullosa, dystrophic
Epidermolysis bullosa, junctionalis, LAMA3
Epilepsy, benign familial juvenile
Episodic falling
Exercise-induced collapse
Factor VII deficiency
Factor XI deficiency
Fanconi syndrome
Fucosidosis, alpha
Furnishings (moustache and eyebrows)
Gallbladder mucoceles
Gangliosidosis, GM1
Gangliosidosis, GM2, type I (B variant)
Gangliosidosis, GM2, type II (Sandoff or variant 0)
Gastrointestinal stromal tumor
Generalized PRA
Glaucoma, primary open angle
Glycogen storage disease Ia
Glycogen storage disease II
Glycogen storage disease IIIa
Glycogen storage disease VII
Golden Retriever PRA 1
Haemophilia A
Haemophilia B
Hair length
Hyperekplexia (Startle disease)
Hyperkeratosis, epidermolytic
Hyperkeratosis, palmoplantar
Hyperparathyroidism
Hypocatalasia
Hypomyelination of the central nervous system
Hypothyroidism
Ichthyosis
Ichthyosis, Golden Retriever
Improper coat
Intestinal cobalamin malabsorption due to AMN mutation
Intestinal cobalamin malabsorption due to CUBN mutation
Krabbe disease
L-2-hydroxyglutaricacidemia
Leber congenital amaurosis (congenital stationary night blindness)
Lens luxation
Leucodystrophy
Leukemia, chronic monocytic
IA 000595-9615 Leukocyte adhesion deficiency, type I
Leukocyte adhesion deficiency, type III
Malignant hyperthermia
May-Hegglin anomaly
Metabolizer of a cognitive enhancer
Mucopolysaccharidosis I
Mucopolysaccharidosis IIIA
Mucopolysaccharidosis IIIB
Mucopolysaccharidosis VI
Mucopolysaccharidosis VII
Multidrug resistance 1
Multifocal retinopathy 1
Multifocal retinopathy 2
Multifocal retinopathy 3
Muscular dystrophy, Duchenne type
Muscular hypertrophy (double muscling)
Musladin-Lueke syndrome
Myasthenic syndrome, congenital
Myasthenic syndrome, congenital, Labrador Retriever
Myoclonus epilepsy of Lafora
Myopathy, centronuclear
Myopathy, Great Dane
Myotonia
Myotubular myopathy 1
Narcolepsy
Nasal parakeratosis
Necrotising encephalopathy, subacute, of Leigh
Neonatal encephalopathy with seizures
Nephritis, X-linked
Nephropathy
Neuroaxonal dystrophy
Neuronal ceroid lipofuscinosis, 1
Neuronal ceroid lipofuscinosis, 10
Neuronal ceroid lipofuscinosis, 12
Neuronal ceroid lipofuscinosis, 2
Neuronal ceroid lipofuscinosis, 4A
Neuronal ceroid lipofuscinosis, 5
Neuronal ceroid lipofuscinosis, 6
Neuronal ceroid lipofuscinosis, 8
Neutropenia, cyclic
Oculoskeletal dysplasia 1
Oculoskeletal dysplasia 2
Osteochondrodysplasia
Osteogenesis imperfecta
Osteogenesis imperfecta_Dachshund
Pancreatitis, hereditary
Periodic Fever Syndrome
Persistent Mullerian duct syndrome
Polycystic kidney disease
Polycythemia
MIA 001917-9615 Polyneuropathy (LPN1)
Prekallikrein deficiency
Primary hyperoxaluria type I (Oxalosis I)
Progressive retinal atrophy
Progressive retinal atrophy type 3, Tibetan Spaniel and Tibetan Terrier
Progressive retinal atrophy, Basenji
Progressive rod-cone degeneration
Pyruvate dehydrogenase deficiency
Pyruvate kinase deficiency of erythrocyte
Renal cystadenocarcinoma and nodular dermatofibrosis
Rod-cone dysplasia 1
Rod-cone dysplasia 1a
Rod-cone dysplasia 2
Rod-cone dysplasia 3
Rod-cone dysplasia 4
Sensory ataxic neuropathy
Severe combined immunodeficiency disease, autosomal
Severe combined immunodeficiency disease, autosomal, T cell-negative, B cell-negative, NK cell-positive
Severe combined immunodeficiency disease, X-linked
Skeletal dysplasia 2 (SD2)
Spinal dysraphism
Spondylocostal dysostosis, autosomal recessive
Squamous cell carcinoma of the digit
Tail, short
Thrombasthenia
Thrombocytopaenia
Thrombopathia
Trapped Neutrophil Syndrome
Tremor, X-linked
Urolithiasis
Vitamin D-deficiency rickets, type II
Von Willebrand disease I
Von Willebrand disease II
Von Willebrand disease III
Wilson disease
X-linked PRA 1
X-linked PRA 2
(Total = 114)
AMP, Alaskan Malamute polyneuropathy
ARVC, arrhythmogenic right ventricular cardiomyopathy
BAER, deafness
BHFD, black hair follicular dysplasia
BNA, Bandera's neonatal ataxia
BTPKD, Bull Terrier polycystic kidney disease
CA, cerebellar ataxia
CC/DE, curlycoat/dryeye
CCN, canine cyclic neutropenia
CD, cone degeneration
CEA/CH, collie eye anomally/ choroidal hypoplasia
CH, congenital hypothyreosis/hypothyroidism
CL, ceroid lipofuscinosis
CLAD, canine leucocyte adhesion deficiency
CM, cobalamin malabsorption
CM/SM, Chiari malformation/syringomyelia scheme
CMHM, BVA/KC CMSM Scheme
CNM, centronuclear myopathy
COMMD1, Copper toxicosis
cord1-PRA, progressive retinal atrophy-cone and rod deterioration-1
cord2-PRA, progressive retinal atrophy-cone and rod deterioration-2
crd3-PRA, progressive retinal atrophy-cone and rod dystropy-3
CSNB, congenital stationary night blindness
CU, cystinuria
DCM, dilated cardiomyopathy
DFM, dwarfism
DM, degenerative myelopathy
ED, ectodermal dysplasia
EDS, BVA/KC Elbow Dysplasia Scheme
EF, episodic falling
EIC, exercise induced collapse
ES, BVA/KC/ISDS Eye Scheme (including annual eye testing)
FN, familial nephropathy
FS, Fanconi syndrome
Fuco, fucosidosis
FVII, factor VII deficiency
FVXI, factor XI deficiency
GCL, globoid cell leukodystrophy
GM1, gangliosidosis
GN, Greyhound neuropathy
GSD, glycogenesis type IIIa
GSDI, glycogen storage disease type I (Pompe's disease)
GT, Glanzmann's thronbasthenia type1
HAVIII, Haemophilia A (factor VIII deficiency)
HBIXl, Haemophilia B (factor IX deficiency)
HC-HSF4, hereditary cataracts
HDS, BVA/KC Hip Dysplasia Scheme
HN, hereditary nephritis
HNM, hereditary necrotising myelopathy
HNP, hereditary nasal parakeratosis
HUU, hyperuricosuria
IC, improper coat
ICT-A, ichthyosis
IRIDA, iron refractory iron deficiency anemia
JE, juvenile epilepsy
JEB, junctional epidermolysis bullosa
L-2HGA, L-2-hydroxyglutaric aciduria
LD, Lafora's disease
LOA, late onset ataxia
LPN1, Leonberger polyneuropathy
MD, muscular dystrophy
MDR1, multiple drug sensitivity/resistance
MLS, Musladin-Leuke syndrome
MPS, mucopolysaccharidosis type VI
MPSIIIA, mucopolysaccharidosis type IIIA
MPSIIIB, mucopolysaccharidosis type IIIB
MPSVII, mucopolysaccharidosis type VII
MYO, myotonia congenital
N/A, No information currently avaliable for this breed
NCCD, neonatal cerebellar cortical degeneration
NCL, neuronal ceroid lipofuscinosis
NE, neonatal encephalopathy
NHPH4, progressive retinal atrophy CRD
NPY, narcolepsy
NTPL1, bitches < 2 yrs not to produce a litter
NTPL2, bitches not to produce > 1 litter in a 12-month period
NTPL3, bitches not to produce > 3 litters in a lifetime
NTPL4, bitches not to produce > 4 litters in a lifetime
NTPL5, bitches not to produce > 5 litters in a lifetime
OI, osteogenesis imperfecta
OSD, retinal/ocularskeletal dysplasia
PCD, primary ciliary dyskinesia
pcrd-PRA, progressive rod cone degeneration -progressive retinal atrophy
PDE, Pug dog encephalitis
PDP-1, pyruvate dehydrogenase phosphate 1 deficiency
PFK, phosphofructokinase deficiency
PH, primary hyperoxaluria
PHPT, primary hyperparathyroidism
PHPV, persistent hyperplastic primary vitreous
PKD, pyruvate kinase deficiency
PLL, primary lens luxation
PLN, protein losing nephropathy
POAG, primary open angle glaucoma
PRA-D, progressive retinal atrophy-dominant
PRA, progressive retinal atrophy
rcd1-PRA, progressive retinal atrophy-rod-cone degeneration-1
rcd2-PRA, progressive retinal atrophy-rod-cone degeneration-2
rcd3-PRA, progressive retinal atrophy-rod-cone degeneration-3
rcd4-PRA, progressive retinal atrophyrod-cone degeneration-4
RCND, renal cystadenocarcinoma nodular dermatofibrosis
SAN, sensory ataxic neuropathy
SAT, sebaceous adenitis testing
SCA, spinocerebellar ataxia
SCID, X-linked severe combined immunodeficiency
SD, Startle disease
TNS, trapped neutrophil syndrome
TPA, thrombopathia
vWD, von Willebrand disease (types 1, 2, 3)
XL-PRA, X-linked progressive retinal atrophy.
AF, anal furunculosis
CMR, canine multifocal retinopathy
GSDII, glycogen storage disease type II (Pompe's disease)
VDD, vitamin D deficiency (Rickets) type 2